A UK-wide survey of healthcare professionals' awareness, knowledge and skills of the impact of food insecurity on eating disorder treatment
01/04/23
Paper synopsis: A UK-wide survey of healthcare professionals' awareness, knowledge and skills of the impact of food insecurity on eating disorder treatment
view the paper: here
Highlights:
- UK eating disorder (ED) healthcare professionals (HCPs) increasingly perceive food insecurity (FI) in their patients.
- HCPs know little about the role of FI in ED onset and treatment and stress the lack of available guidance resources.
- HCPs welcome resources on integrating FI into ED care and support introducing routine FI screening in ED services.
- HCPs also expect other cost-of-living crisis driven issues to increasingly impact their patients.
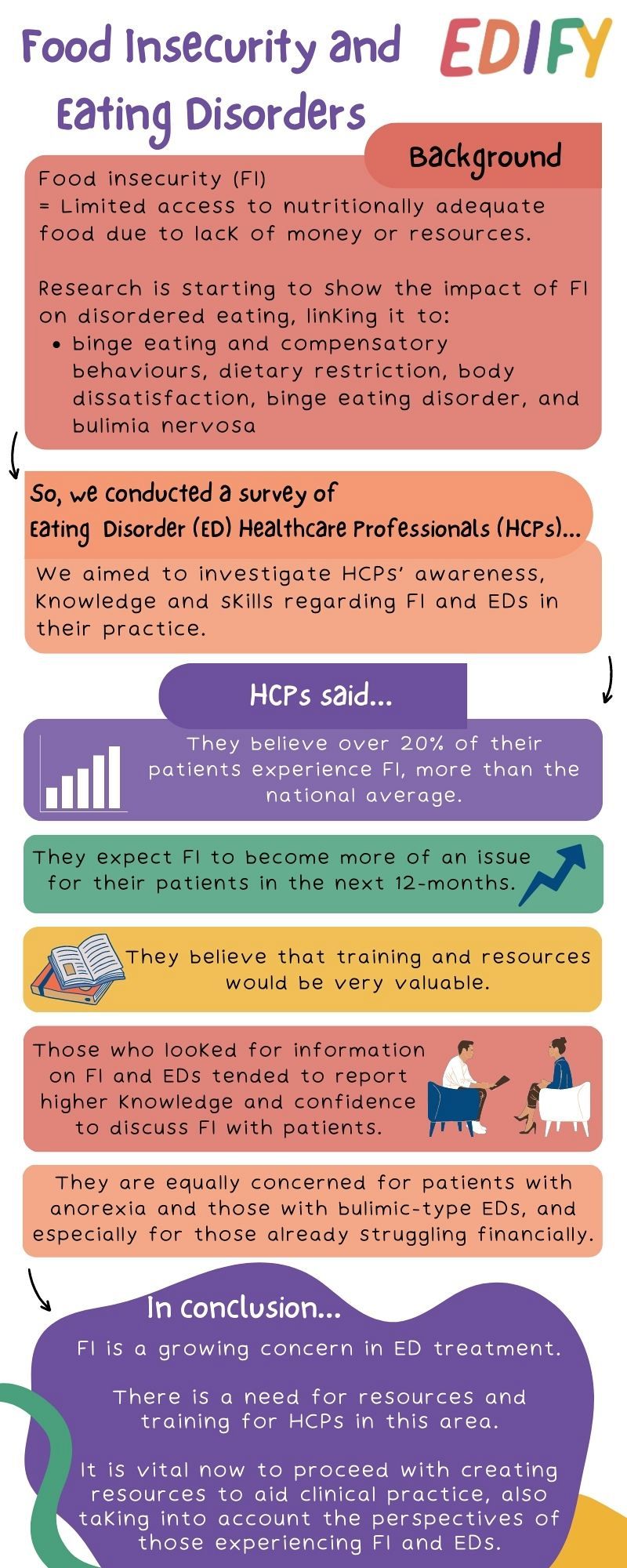
Food insecurity (FI) has a significant negative impact on health and wellbeing. The UK is currently experiencing a cost-of-living crisis, and FI is on the rise. FI has been linked to disordered eating behaviours, such as cyclical over- and under-eating depending on food availability, and recent findings suggest an association between FI and diagnoses of binge eating disorder and bulimia nervosa. The majority of studies have focused on non-help-seeking populations, so little is known about the impact of FI on ED treatment. The current study explored the impact of FI on eating disorder clinical practice in the UK, aiming to assess healthcare professionals’ (HCPs) knowledge, skills and views on the topic of FI in their patients.
We circulated a 15-item survey, with rating and open-ended questions, to ED professional organisations in the UK. 93 ED HCPs completed the survey, and we used descriptive statistics to examine and summarise the quantitative data. We used descriptive content analysis to examine the free text answers to open-ended questions.
We collected a variety of information from HCPs, including profession, index of multiple deprivation (IMD), self-reported perceived deprivation of the work area, years working in the ED field, healthcare sector, and previous training on FI.
Results:
- On average, HCPs reported that they perceived more than a fifth of their patients to have experienced FI in the past 12-months
- HCPs anticipated FI to likely become an increasing issue over the next 12-months (M = 61.08, SD = 29.07; scale from 0 [extremely unlikely] to 100 [extremely likely]).
- HCPs believed that training and resources would be very valuable (M = 87.67, SD = 18.69; scale from 0 [definitely not valuable] to 100 [definitely valuable]).
- Those who looked for information on FI and EDs tended to report higher knowledge and confidence to discuss FI with patients.
- HCPs expressed concern equally for those with anorexia and those with bulimic-type EDs, and especially for those already struggling financially.
In conclusion:
- Food insecurity is a growing concern in ED treatment.
- There is a need for resources and training for HCPs in this area.
- It is vital now to proceed with creating resources to aid clinical practice, also taking into account the perspectives of those experiencing food insecurity and EDs.
Share
